Several decades ago a South African leader at his trial: "There is only one race: the Human race." No it was not Nelson Mandela, although he would have agreed wholeheartedly. It was Robert Sobukwe. He was imprisoned on Robben Island in solitary confinement because his views so directly undermined and threatened the very existence of Apartheid.

Apartheid is based on the lie of racism.
There is no scientific justification for race classification at all. This was recently demonstrated by a
National Geographic cover of twins who appear to be of different races but who have the same parents and were born on the same day. Racist attitudes and colonial notions of racial superiority were reinforced by Darwin who gave Hitler's master race ideas the veneer of scientific legitimacy. So too the ideas behind Apartheid and the notion of "separate but equal" races were built on this odious lie.
The fact of the matter is that every human being on the planet comes from the same gene pool, and this upsets a lot of the anti-colonial rhetoric that says that "settlers" from Europe are not African and are therefore not welcome. The fact of the matter is that we are all African.

Those of us who opposed Apartheid did so because we knew that racism was wrong and ungodly. Man is created in the image of God, and this applies equally to all human beings. People like Beyers Naude endured a lot of persecution in his own church because he told them that Apartheid was a heresy and the church needed to repent of its racism and support for Apartheid. People like Desmond Tutu and Trevor Huddlestone spoke out against the injustices of Apartheid, including crimes against humanity like Forced Removals, job reservation and unequal education. One of the common themes among all anti-Apartheid groups and organisations was the notion that we were fighting for a non-racial South Africa, where the colour of one's skin no longer played any part in the life of the nation.

We wrote into our Constitution that "South Africa belongs to all who live in it" because we were conscious of how many people in the past were evicted from their homes or treated as unwelcome in the country of their birth. We abolished the Population Registration Act and removed the digits in the South African ID number that indicated our race. We elected our first truly democractic President Nelson Mandela, who repeated over and over that the South African government was working for ALL South Africans. Until it wasn't.
"Go back to your Homeland"

Somewhere along the line our politicians started focusing once again on race. Not just blaming all their current mistakes on racism and Apartheid and our colonial history, but using racist solutions to attempt to rectify racist problems. The more they felt the heat for their incompetence and corruption, the more they started beating the race drums, stirring up racial tensions and promoting Xenophobia. some of them colluded with PR agencies to come up with rhetoric about "White Monopoly Capital", while others just incited riots against Somalis, Kenyans, Mozambicans, Zimbabweans, and Nigerians, who they claimed were "introducing crime" or "stealing jobs" from local people.

The sad fact of the matter is that generally immigrants are more willing to work harder for lower wages and longer hours than the local residents, who feel "entitled" to cushy jobs that magically appear from nowhere. They see how lazy civil servants get away with poor performance and think that is the norm. I spoke to a hotel manager who wanted to employ locals within walking distance of his hotel, but gave up because they were lazy and unreliable. He employs people whose homes are hundreds of km away, but who are grateful for the job and willing to work. The salary and working conditions are the same, just the attitude is different. And they all live within the borders of the country.

You know things are getting bad when Somalis start talking about returning to their war-ravaged country rather than put up with the xenophobic hostility here. The ANC and PAC were given shelter and support by African countries almost without exception, yet we repay their support of our struggle by murdering their refugees.
Job Reservation and Race

Our constitution guarantees equal rights for all, yet our government thinks that this must be achieved by manipulating race quotas in industry to ensure that "previously disadvantaged communities" are given more opportunities. This noble idea is translated to crude race classification and jobs for pals as follows: companies must come up with "Employment Equity" quotas, and employ people accordingly, or face fines and other sanctions. So it boils down to employing more black people, assuming you can find candidates suitably qualified for the job. Of course this leads to the "chicken and egg" problem because where do you find experienced people unless someone else employed them first?

So you end up having to employ someone black who isn't experienced at the same salary as an experienced person. Until the new employee gets the hang of the job and doesn't make too many costly mistakes, their salary is costing the company money. So the company has to decide whether to run the risk of being fined, or run the risk of overpaying an inexperienced person instead. Big companies can absorb the slack, smaller companies can't. Often the companies that do take the risk of employing a black manager are rewarded by the person leaving after a year or so because they are offered a better paying job somewhere else by another company more desperate for the "right" employment equity numbers.

So during Apartheid we had jobs reserved for particular races. Now we have a different focus on the racial makeup of a company, but its racial nonetheless. It extends to the ownership and shareholding of the company too. Companies who supply services to government have to be "BEE Compliant" and are encouraged to have Broad-Based Black Economic Empowerment (BBBEE) credentials as well. Black Economic Empowerment (BEE) was supposed to be a short term fix to address the racial inequalities of the past. It's now permanent, so that job seekers born after 1994 entering the workplace are puzzled and insulted to be asked what their race is.

Not only when they go for a job interview, but when they apply to any educational institution they have to provide their race, gender, nationality, disability status and residence status on the application form. Any institution requiring accreditation needs to be able to provide these figures to the Council for Higher Education twice a year. I was given the odious task of extracting and collating this data for one of my clients. The CHED claims it is for statistical purposes only, but they can remove the accreditation from any institution they think is being racially exclusive. To hell with the rights of the students: they must just suck it up and be forced to disclose their "race" even if they don't like it. They can't answer "100m" or "human" when asked for their race.

In government there is also the concept of Cadre Deployment, another term for "jobs for pals" or "jobs for sale". There are plenty of documented cases of people desperate for jobs who have to bribe a party or union official to be considered for a job. Never mind exploitation of the poor, self-enrichment is far more important.
State Owned Enterprises

The Apartheid government not only embraced the racist ideology of the Nazis, but the economic ones as well. They used National Socialism as a means to build the country and employ as many white Afrikaners as possible. As an English-speaking white person I was never included in the "
Volk en Vaderland" when it came to jobs or political influence, but I was expected to put my life on the line to "defend" the country from "communists", even if they were English-speaking communists like Joe Slovo or Peter Hain. They developed the Post Office to provide postal and telephone services, the South African Broadcasting Corporation to provide radio entertainment and propaganda to counter the opinions in the newspaper industry, ISCOR to make steel, the South African Railways and Harbours to provide transport, SANRAL to maintain the roads, South African Airways and The Airports Company to look after aviation, and so on. SASOL devised a way of turning coal into a petroleum industry, which was most useful to counter sanctions, and ESKOM used coal and other technologies to generate electricity.

The ANC, being the ruling party and liberation movement, decided that these State Owned Enterprises (SOEs) were a great place to provide jobs for pals and contracts for party members. In their infinite wisdom they also decided that South Africa wouldn't need any new power stations (until suddenly it did) and so we experienced "load shedding" which led to "job shedding" until the demand for electricity dropped to meet the inadequate supply. ESKOM was never that efficient to start off with, but it is now bloated with far too many employees earning far too much money and producing far too little. The country simply cannot sustain the level of incompetence and looting that has been going on in the SOEs, hence our credit downgrade.

Few if any of the SOEs make a profit any more, and the ones that are profitable are largely run as business enterprises and not government departments. One of the big complaints during Apartheid was that government departments simply didn't care about ordinary people, and were bloated and ineffective. The people in those departments and SOEs may have changed, but the results are exactly the same.
Bantu Education

The Apartheid regime spawned an inferior education system for blacks. The idea was to provide only basic literacy and a strong emphasis on punishment and discipline. It was such a glaringly obvious injustice that everyone opposed to Apartheid agreed that the system needed to change. The South African Democratic Teachers' Union (SADTU) organised among teachers and campaigned for an end to the "Education Crisis" in SA schools. When the ANC took over the running of the country in 1994 it was no surprise that they wanted to make changes to the education system. But they threw the baby out with the bathwater, closing down all the "Bantustan" teacher training colleges instead of upgrading them. Then they introduced Outcomes Based Education (OBE) that was so badly implemented that it ruined the education of a decade of children.

In the meantime SADTU gained influence in the education departments and started a system of patronage, where teachers would have to PAY union officials for posts in schools. Even after OBE was abandoned, the decline of the education system continued. Not just the teaching quality (rural schools spend half as much time on average teaching as urban schools) but the logistics too. School textbooks found languishing in storerooms, children being taught under trees because the buildings were dilapidated or burnt down, and pupils drowning in pit latrines. The liberation movement that had the slogan "liberation before education" now continues to fail the children of today with poor education quality, ineptitude, mismanagement and corruption. One gets the impression that the ANC wants to keep the population ignorant, unemployable and dependent on the state for everything. A good way to retain votes, but at what cost to the stability and future of the country. Instead, we need to be teaching our children "I am a job creator not a job seeker".

Forced Removals

One of the worst excesses of Apartheid was the notion that people should live in different areas based on their race. Not only within homelands, but every
platteland dorp or town has a township down the road that is economically dependent on the town for municipal services, shops and jobs, but houses most of the people. It will take a while for this to change, but so far all we have managed to do is make most of the municipalities go bankrupt and provide even fewer services than before. Many private sector businesses dependent on municipal services like water and electricity have closed too, and their owners have sought better opportunities in bigger towns or cities.

Just when things couldn't get any worse, the ruling party decided to change its tune on land ownership, all in the name of "Radical Economic Transformation" which is best described as racial socialism. They have decided that since the land redistribution process has "failed", they need to force the issue by expropriating land without the obligation to compensate the owner. Never mind that the government has a bigger budget for VIP protection than land redistribution, or that 90% of all farms transferred to their new black owners have failed to remain productive. So the new landowners end up starving or growing subsistence crops only. One or two exceptions have been trumpeted in the media, but most expropriated farms are still owned by the state and are in a shambles.

Expropriation Without Compensation makes a bad situation worse, because it leads to the financial ruin of the person being expropriated, and forces him off the land. Exactly the same as forced removals. The Apartheid regime expropriated land from white farmers to "consolidate" homeland boundaries, and in some cases they forcibly evicted these farmers, but they were at least compensated to some extent. Black victims of forced removals weren't given a cent.


Now the political rabble-rousers have come up with a fresh round of racist propaganda stating that ALL land in South Africa was STOLEN from the original BLACK inhabitants of the land by WHITE SETTLERS. Not only is this racist bullshit completely unscientific, but it is historically inaccurate as well. Add to this the inconvenient problem caused by physics: the perpetrators of these "crimes" are long since dead. So their "crimes" are visited on their "descendants" both real and imagined. A new state is granting itself the power to uproot a new bunch of people (mostly framers to begin with, but it won't end there) and toss them off their property without compensation. No one has explained what will happen to their bonds with the bank, or how they will be compensated for the buildings and improvements they may have made to the land. That is all drowned in the angry voices demanding retribution for the sins of the past, and providing justice for no one.
Entitlement and Privilege

I grew up in a country where my skin colour entitled me to various benefits and privileges. This was tempered by my parents and grandparents who taught me that racism was wrong and I should treat everyone with respect. My dad started in a lowly job on the gold mines and he slowly rose through the ranks until he was a mine manager. He was determined to provide me and my two brothers with a private school education, even though he could have used the money for fancy holidays and sent me to a state school. So I was able to get a university education, something he never had. But together with this privilege came responsibility. I felt responsible for the good running of the country and the economy, and for the plight of the people who were being deprived in their own country.

When I arrived at Natal University and realised that the problems were much bigger than I thought, I was forced to make hard choices about right and wrong, and I refused to serve in the Apartheid military, since I could not justify the killing of another human being, let alone someone from my own country.

Today on social media there are a lot of shouting angry voices who (wrongly) assume that ALL WHITES are racist, and that if your name sounds "white" then you must have been a supporter and beneficiary of Apartheid and therefore you must shut up and sit down and not say a word. You are no longer welcome here. Never mind "South Africa belongs to all who live in it", you must just leave your money behind and go back to wherever your settler ancestors came from. Such hatred and bitterness will hardly improve the lives of anyone, except the looting leaders who will keep looting until it's all gone.

They fail to realize they are being manipulated by greedy leaders who want to retain their power by blaming their failures on others. During Apartheid the problems were all blamed on the "communists" and "agitators" (i.e. people who speak English) who "stirred up the blacks" into "black-on-black violence". Now all our problems are blamed on "Apartheid racism" and the "colonial legacy" (i.e. people who speak English). Now we must "decolonise" our universities (i.e. get rid of the white lecturers) and engage in "economic transformation" (i.e. employ more blacks in a diminishing number of jobs) while chasing away the "colonial settlers" who brought the jobs in the first place.

It seems that
all rationality and good sense is being thrown out of the window. Welcome to Apartheid 2.0

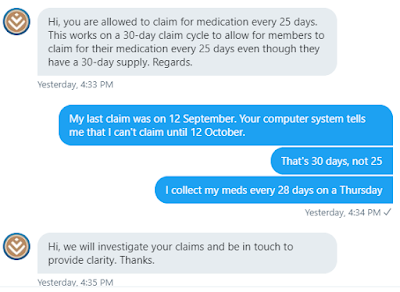
The law states that not more than 1 month supply of a medication can be provided at a time – these are the “prescribed conditions” that take the interval between prescriptions into consideration as well as the maximum registered dose per days of supply. We electronically enforce monthly prescription refill rules to accommodate the legislation within a reasonable claiming period i.e. 23 or 26 days instead of 30 days.
The onus is still on the pharmacist to ensure that legal prescription refill intervals are enforced. If this is not done, we have additional quarterly and annual validation rules that ensure we do not reimburse in excess of routine allowable prescription filling rules.
For example, the pharmacist can submit 13 fills for 30 tablets in a 12-month cycle and our system will allow you to claim every 23 days instead of waiting for 30 days (4 fills in 90 days). Should there be a discrepancy in which the quantity submitted on a claims doesn’t match the number of days of therapy submitted on system, this might cause the system to reject the claim. However in those instances, the pharmacist can call our Propharmaceutical Benefit Management Department to get clarity on the rejection and check if a possible override can be done
If you have any more questions, please visit www.discovery.co.za to log a query or call us on 0860 99 88 77.