Update noon 22 July: common sense and decency has prevailed and "the committee" has decided that they really don't need to see a photo of my arse after all. See
Dr Martin Young's take on the matter
here.
 Discovery Health
Discovery Health is a medical "aid" with some weird ideas. Once of them is that they claim to practice "evidence based" claims processing. This has some weird side effects, such as their latest debacle: they want a photo of my injured backside. First, some background.

On Friday 26th June I noticed that a lump on my left buttocks was getting swollen and painful. On Saturday it got worse and eventually I decided to go to my GP for treatment. By then their offices were closed and I was directed to the
Olivedale Hospital instead. Their emergency doctor identified a peri-anal abscess and used a local anesthetic while she made an incision to drain the pus. I was then given antibiotics, pain killers and a dressing and told to come back on Monday for a checkup.

It was still painful on Monday and my GP took one look at the wound and said I needed to see a specialist surgeon at Olivedale. On Tuesday I saw the specialist surgeon who examined me and said I needed surgery as soon as possible and antibiotics on a drip. I was to report back to the
Olivedale Hospital later that evening and he would operate the following morning, Wednesday 1st July.

The necessary hospital pre-authorization was obtained from
Discovery Health, and I took a printout of the authorization number 17263206 with me. Because the surgeon also wanted to do a follow-up colonoscopy, I had to make a "co-paymnent" of R2750 when I got to the hospital. The pre-authorization email ended with a curious statement:
You can receive the care you need at home with Discovery HomeCare
Discovery HomeCare is a unique healthcare service that offers our members quality home-based care in the comfort of their home. Certain treatments can be rendered in a home environment, making it possible for Discovery HomeCare to provide quality nursing and care worker support in your home rather than in in a medical facility or institution. For more information on Discovery HomeCare visit our website www.discovery.co.za.
If you are interested in this service, please discuss this with your treating doctor. If your doctor is in favour of you receiving care at home for your condition, please email or call us on 0860 99 88 77.
We hope this information helps you prepare for your hospital stay.
When you read that does it sound like you need to obtain pre-authorization for the
HomeCare? Does it imply that the doctor has to send
Discovery Health a motivation letter and photos before the care commences? It is sufficiently vague as to not even specify the email address to contact. Even the website address is very generic and non-specific. I have provided a link to the relevant page. But I digress.

I was admitted on Tuesday evening and after some confusion put in a ward and given a drip. This contained antibiotics and pain killers. The surgeon and the anesthetist came to see me and asked me various questions to establish my past medical history and so on. On the Wednesday I was given a general anesthetic at around 11am and when I woke up they had drained the pus completely and I had a large hole in my backside with gauze in it to prevent the wound from closing. I continued to receive antibiotics and pain killers via the drip for the rest of Wednesday and Thursday morning.

The following day the dressing was changed (quite painful) and I was allowed to go home on Thursday afternoon. The surgeon introduced me to a private nurse who would come round to my home on Friday and on the weekend to dress the wound and make sure the infection did not come back. There is a 20% chance of the abscess recurring. I was quite keen to avoid going through this process again.

I couldn't sit down properly on Friday or Saturday, so work was out of the question. I was advised to take at least 2 weeks off work. Since I am self-employed this wasn't difficult to arrange. Those first few dressing changes were painful, as the gauze went quite deep into the wound, where there are plenty of nerve endings. I was given stuff to put in the bath, and had to soak the would before the nurse arrived. By Monday I was able to walk outside and on Tuesday I decided to try going to the gym to see if I could manage any exercise. The sweat made the wound itch, but apart from that I managed fairly well.

I was also able to catch up on some admin work so I sent in the motivation letter provided by the private nurse, as well as the first invoice, which I had paid.
Big mistake, according to
Discovery Health.
I shouldn't have sent the motivation letter along with the claim to
claims@discovery.co.za, which seemed to me to be the logical thing to do.
What I was supposed to have done, according to two different
Discovery officials I spoke to today, is to have phoned
Discovery when I got home, and requested permission to be treated by the nurse, even though the surgeon had already told me that he required it to be done. Then I was supposed to obtain a motivation letter from the nurse and the surgeon and send them to
preauthorisations@discovery.co.za and wait for a response.
"If your preauthorisation request does not need additional input, we will get back to you in 2 – 3 working days. For requests that need additional review, we will give you feedback in 3 – 5 working days."
Never mind that the wound would probably have gone septic by then. But then
Discovery Health doesn't provide health care: they are only accountants and insurance providers who try to avoid paying for it whenever they can. They have the audacity to call themselves a medical "aid". Perhaps "Medical Scheme" is more accurate, but it doesn't identify who does the scheming.

Treatment continued from 3rd July to 13th July, and I submitted claims as I paid the invoices. Each time I sent the motivation letter along with the invoice and receipt to
claims@discovery.co.za. And each time I received an automated notification that my claim was being processed. No mention that the motivation letter was being sent to the "wrong" address. After all,
they only process claims, and I am supposed to know how their system works. I'm the customer who pays, remember?

Today (Friday 17th) I noticed that my claim refunds were being deducted from my Medical Savings Account, and not being taken from the much-vaunted Hospital Benefits, even though the hospital, anesthetist and surgeon were all paid from the Hospital Benefit. So I called to find out. That's when things got a bit bizarre.

Firstly, I was told that the claims department doesn't decide which claims should come from Hospital Benefits, only the pre-authorisation committee can do that, and they were still busy with their decision. They promised to escalate the request, since it was now 10 days since I had sent the letter. At 16h22 on Friday they sent me the following letter:
Dear Mr Edwards
Request for Wound Care for Mr Donn Edwards
Thank you for your recent communication to Discovery Health.
We have received your request for Wound Care from Sr Bev Lawrence. In order for us to assist you with this request. We require the following information:-
- A detailed Letter of Motivation from the requesting Doctor indicating the clinical information of the wound.
- A quote with the relevant nappi codes.
- A recent colour photograph of the wound with a ruler indicating the size of the wound, patient details and date. Photographs need to be submitted in a JPEG, PDF, PNG , GIF, DOC , DOCX format to be viewed in colour.
- The exact treatment dates.
Please send the information to us by:-
Fax: 011 539 2192
Email: preauthorisations@discovery.co.za
I trust all of the above is clear and to your satisfaction; should you have any further questions in this regard, please do not hesitate to contact Discovery Health.
For any queries send an email to clinicalhelp@discovery.co.za or visit www.discovery.co.za
Regards
Orleans Ledile Sindane
Discovery Health (Pty) Ltd
On behalf of Discovery Health Medical Scheme
Both the surgeon and the nurse had warned me they might try a stunt like this, and absolutely and point blank
refused to be associated with any photographs in any way. I have yet to figure out how to take a selfie of my own backside. The letter refers to National Pharmaceutical Product Index (NAPPI) codes. These are a unique identifier for a given ethical, surgical or consumable (pharmaceutical) product, not for treatment procedures. Treatment procedures are identified by ICD codes, K61.3 and Z48.0. So presumably when they say "we have received your request" it means that have only
received it, but not actually
read it.

I still can't believe they could actually send a letter like that. Especially the bit where I am supposed to
fax them a
colour photograph or my backside. Seriously? So I replied as follows:
Dear Orleans Ledile Sindane
I fail to understand your request, late as it is. Specifically:
a) The wound has almost completely healed, a photo is a little bit late, don’t you think?
b) The wound area is close to my anus. You have no right to request a photo of a private area such as this.
c) The photo cannot be taken by either the doctor or the nurse without them being prosecuted for privacy violations, since the injury is in my anal area. You would know this if you had bothered to read and comprehend Sr Lawrence’s letter (attached)
d) Sr Lawrence provided both the ICD 10 codes and a quote. See attached letter.
e) Sr Lawrence provided measurement information of the size of the wound in her letter.
f) Treatment commenced on the day after I was discharged from Olivedale Hospital (i.e. it began on 3rd July 2015) and concluded on 13th July 2015. You already have these dates because I have sent all the invoices from Sr Lawrence to claims@discovery.co.za. I have attached them again anyway for your easy reference.
So if I understand matters correctly, you require a motivation letter from the surgeon at Olivedale. Have you informed the surgeon, or do you expect me to waste more time going to see him to obtain such a letter?
Kindly advise
Donn Edwards
This raises a number of ethical concerns. Just who exactly gets to look at sensitive photos of my backside? The fact that they are happy for me to email them means that they have
no concerns whatsoever about security or privacy, since emails of this nature can be forwarded to anyone they like, and their is no audit trail. Also, the emails are not secure, and we know for a fact that both the GCHQ in the UK and the NSA in the USA have copies of all emails sent in the last few years, including ones in South Africa. I may as well just post the photos on Twitter. Twitter messages are just as confidential as email, i.e. not at all.

What gives a bunch of accountants the right to request photos of my body? If they have already paid for the surgeon to operate under general anesthetic,
they know that there will be a post-operation wound. Why do they need a letter from the surgeon and the nurse, as well as photos? Why not the anesthetist as well? Don't they believe the doctor and/or the nurse?
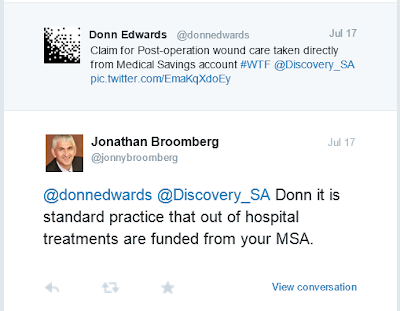
Update Saturday 18th July 2015: I have been assured by
Jonny Broomberg via
Twitter that only qualified health care professionals will see the information. I find this difficult to believe, given the nature of email. I find it more disturbing that a "health professional" would even request such a photo in the first place. What kind of perverts are they?
Then there is the question of the way the refunds are being financed. They are "borrowing" money from my Medical Savings Account for the purpose, i.e. it isn't covered by the Medical Scheme benefits. The money in the MSA is my money. It doesn't belong to Discovery. Nice of them to pay it back to me instead of paying it out of my hospital care benefits. This is the first time I have been to hospital since 1986, so its not like the funds are depleted or anything.
Even Mr Broomberg seems to think this is OK. He's a member of the
Social and Ethics Committee and CEO of Discovery Health
He obviously thinks that "post-operation wound care" is an "out of hospital treatment". I disagree, but them I'm only the paying customer, so I must be wrong.
Update Monday 20th July: I called
Discovery Health and spoke to someone at the pre-authorizations call centre. She confirmed that email confidentiality cannot be guaranteed by Discovery Health, nor that only qualified healthcare practitioners would see the photograph.

Since she was unable to help me resolve the issue, I was put through to Danette, since Orleans Ledile Sindane wasn't available. Danette explained that the
photograph requirement is non-negotiable, but isn't written in the Member Rules, so there is no way that I would be able know about this in advance. He also accused me of
being irresponsible for not phoning Discovery
after being discharged from hospital. When I pointed out that her insistence on a photograph was effectively blackmail, she wouldn't back down. I asked her to repeat her insistence in writing. Here is her letter:
Dear Mr Edwards
Thank you for contacting us.
Request for conservative wound care
As per the communication sent to you on 17 July 2015 we informed you of the information we require in order to review the conservative wound care from the Hospital Benefit.
We received confirmation from you and Sr Bev Lawrence that you are not willing to send colour photos to Discovery Health for review. We are therefore unable to confirm funding from the Hospital Benefit. The claims will be funded from your available Day-to-Day Benefit as per your chosen plan type and the Discovery Health Scheme and billing rules.
We make consistent and fair funding decisions in the interest of all Scheme members
We recognise that treating provider is in the best position to make medical decisions about your condition and treatment. In reaching this decision we have not questioned the diagnosis or the treatment recommended by the treating provider. As a healthcare funder, we decide on funding treatment to make sure the Scheme can cover claims now and in the future.
Our role is to make sure members of the Scheme enjoy access to quality healthcare in a way that remains affordable and sustainable.
Some of the ways we achieve this is in our plan and benefit design, the creation and application of funding policies and clinical protocols that are developed using a rigorous, evidence-based decision-making process. This process also helps us make decisions about which procedures and treatment to exclude from cover.
If you have any more questions, please call us on 0860 99 88 77, email clinicalhelp@discovery.co.za or visit www.discovery.co.za
Regards
Danette Gerber
Discovery Health (Pty) Ltd
On behalf of Discovery Health Medical Scheme
That's a nice way of blackmailing me: no photo, no benefit. The red emphasis is mine.

Also, on Friday I asked the
Discovery CEO whether he would be prepared to take the photo of my backside. He's ducking and diving and won't reply. He knows it's illegal and doesn't want to run the risk of losing his license and landing up in jail.
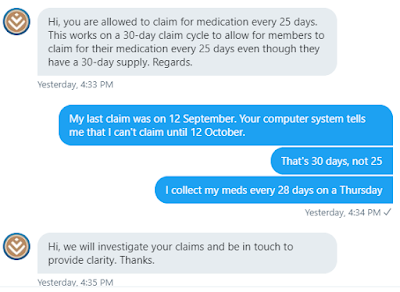
I also tweeted that I thought
Discovery was blackmailing me. Their replies show their hypocrisy and lack of understanding of the nature of reality:
I proposed a different solution: I would come in to their offices and show the photograph directly to a qualified healthcare professional. They can't do that because the "Benefits Committee" meets electronically. So they have to have an electronic copy. There is
no secure upload facility on their web site, and they admit that a fax copy isn't in colour, so I have to send it via email.
This is how seriously they take the confidentiality of their medical information.

The
Twitter PR guy seems to think its OK for me to bring the photo to their walk-in centre.
Update Tuesday 21st July: Last night Jonathan Broomberg emailed me and asked if it was OK if Discovery's team could talk to my surgeon and the nurse. I said this would be most welcome and supplied him with their numbers. It seems like sanity and common sense may yet prevail. I hope so.
In the meantime, my friend
Dr Martin Young has written
an insightful article on the matter for his own blog.
Update Wednesday 22nd July: Three weeks after the operation, and 2 weeks after submitting my claim for post-op care, it has taken the personal intervention of the CEO to get "the committee" to decide that they don't need to blackmail clients and insist on a photo if it offends medical and social ethics. They just phoned me to confirm that they will indeed cover my post-op care from my hospital benefits and not out of my own pocket.

To the trolls on
Twitter who claim I made this all up to defraud my medical aid: I am waiting for the day you get a very painful infection and have to hear your medical aid administrators tell you that they won't cover it. Then all of a sudden you'll think a little differently about what should be covered or not.

And in any case, I had to pay the money from my own account and then wait for a refund. I made nothing out of it financially. The nurse provided a medical service and didn't prolong the treatment for a day longer than necessary. She charged Medical Aid rates and didn't charge for the plasters and gauze, because it was already supplied by the hospital pharmacy.

The nature and position of the wound was such that I can't see it or treat it myself, not even with a mirror. And it was too painful to allow an amateur to touch it. That's why I had to have a general anesthetic for the initial operation. DUH!
Discovery's risk analysis people are clever enough to realize that providing post-op care by a professional is better and cheaper than (a) keeping the patient in hospital for 2 extra weeks and (b) forcing the patient to do the dressing himself (assuming he can actually reach the injured part) and running the risk of the wound going septic. There is in any case a 20% chance of the abscess returning. Halving those odds will reduce their hospital costs considerably. Prevention is better than cure in many ways.

When the smug Discovery PR person phoned to explain their procedures and pointed out that I should have known in advance that I was supposed to obtain pre-authorization or post-op care, I said to him that I thought
he was exactly right, and that that made me feel much better about his company and I was most likely to recommend them to all my friends because they had proved that
they were right and I was wrong. I don't think he got the sarcasm.

Neither their web site nor their emailed letter to me said anything
about obtaining permission or authorization in advance. It still doesn't. It makes general hints and relies on the customer to call and find out. Why they
can't be open and upfront in advance I don't know. Perhaps a paragraph like this would help:
We want you to get better after your operation, so before you leave the hospital you need to obtain permission from us to get better. In order for us to grant such permission, we'll need a quote from the nurse, and a motivation letter from the referring doctor, together with a detailed description of the wound, photos of the wound with an electronic date included and a ruler or tape measure blocking any private areas, a list of all the plasters, ointments, medication and pharmaceutical products to be consumed.
We'd prefer not to have to pay for this so if you can treat the wound yourself, tough luck and we hope you get better on your own. Remember that without prior approval for such treatment, which we don't see as in any way related to your recent stay in hospital, you will have to pay the bill yourself out of your own funds.
We think you are just using your hospital stay to milk us of all your monthly contributions and make a profit at our expense. Sorry, buster, we make the profit and keep 15% of your money no matter what else happens.
The problem is that companies and institutions set up systems with their own (evil) logic and rules. The people inside those organisations don't see how these rules clash with reality. They'll ask for a photo taken two weeks ago without even thinking about the laws of physics. They'll instruct a nurse to do something unethical for which she could go to jail, and then not understand why she refuses.

Most of us just capitulate because it's too much hassle to kick up a fuss. I kicked up this fuss because my butt was on the line. Hopefully now others will have a more compassionate experience. I'm just glad it wasn't my previous medical "aid". I left them in 1999.